Description
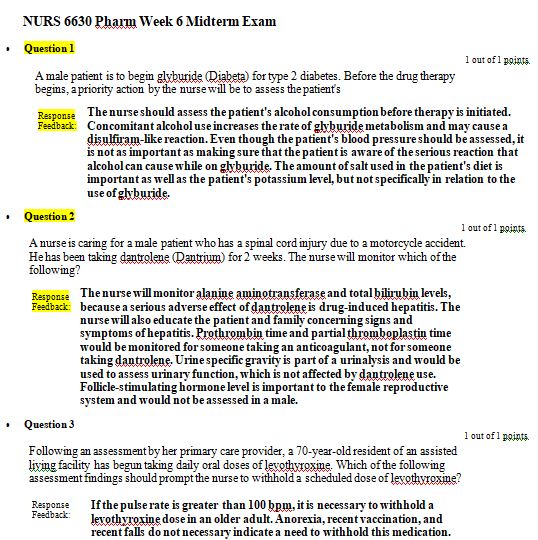
NURS 6630 Midterm Exam Pharm Week 6
- A male patient is to begin glyburide (Diabeta) for type 2 diabetes. Before the drug therapy begins, a priority action by the nurse will be to assess the patient’s
- The nurse should assess the patient’s alcohol consumption before therapy is initiated. Concomitant alcohol use increases the rate of glyburide metabolism and may cause a disulfiram-like reaction. Even though the patient’s blood pressure should be assessed, it is not as important as making sure that the patient is aware of the serious reaction that alcohol can cause while on glyburide. The amount of salt used in the patient’s diet is important as well as the patient’s potassium level, but not specifically in relation to the use of glyburide.
- The nurse will monitor alanine aminotransferase and total bilirubin levels, because a serious adverse effect of dantrolene is drug-induced hepatitis. The nurse will also educate the patient and family concerning signs and symptoms of hepatitis. Prothrombin time and partial thromboplastin time would be monitored for someone taking an anticoagulant, not for someone taking dantrolene. Urine specific gravity is part of a urinalysis and would be used to assess urinary function, which is not affected by dantrolene use. Follicle-stimulating hormone level is important to the female reproductive system and would not be assessed in a male.
- If the pulse rate is greater than 100 bpm, it is necessary to withhold a levothyroxine dose in an older adult. Anorexia, recent vaccination, and recent falls do not necessary indicate a need to withhold this medication.
- Dantrolene causes weakness because of its generalized reduction of muscle contraction. It is not associated with drug dependence, hyperglycemia, hypoglycemia, or hallucinations.
- Gabapentin is not metabolized and is excreted unchanged in the urine. Therefore, it is important to monitor renal function. Hepatic, cardiac, and respiratory functions are not compromised with this drug.
- Subcutaneous insulin therapy for type 1 diabetes frequently consists of daily injections of mixtures of short-acting regular insulin with intermediate-acting insulins; multiple doses of regular insulin before each meal in association with one or two daily doses of long-acting insulin may also be used. Frequent, fixed doses of rapid-acting or intermediate-acting insulin may result in unsafe blood sugar levels.
- The nurse should ask the patient to report immediately if he notices decreased cardiac rate, intolerance to cold, or weight gain. These are indications of hypothyroidism resulting from antithyroid therapy, and if the medication is continued unchanged, insidious goitrogenic hypothyroidism may occur. Vertigo, drowsiness, loss of appetite, and epigastric distress are possible adverse effects of the therapy but would not present an immediate risk to the patient’s health.
- Gabapentin is unusual in that it does not interact with other drugs and does not alter the serum concentrations of other anticonvulsants. Consequently, it is unnecessary to modify the patient’s existing drug regimen. Regular assessment of renal function is necessary in patients with diabetes, but this is not a consequence of the use of gabapentin.
- Special instructions need to be given to patients with diabetes when they are prescribed syrups. A diabetic patient needs to monitor glucose levels closely because syrups contain high levels of sugars, which can cause elevated glucose levels. Increased gastrointestinal tract infections are not directly related to diabetic patients taking cough syrups. Noting the time that a medication is taken and good hand-washing are always important, but are not specific considerations for a diabetic patient taking cough syrup.
- The nurse should teach the patient to take each dose after a meal to decrease the potential for nausea and vomiting. Taking this medicine at night, in the morning, or before a meal would not help decrease the GI symptoms associated with this drug.
- During long-term ibuprofen therapy, especially in patients older than 60 years, the nurse needs to closely monitor for peptic ulcer disease or gastritis that can lead to gastrointestinal bleeding or even bowel perforation. These events can occur at any time, with or without warning. Ibuprofen may also cause excessive or abnormal bleeding, especially in patients with anemia, but it is not known to cause anemia. Interstitial nephritis is one of the less common renal toxicities associated with ibuprofen as is constipation.
- Somatropin is used for the long-term treatment of pediatric patients who have growth failure due to an inadequate secretion of endogenous growth hormone; therefore, the nurse should check the patient’s height. If the patient’s growth rate does not exceed the pretreatment rate by at least 2 cm per year, nonadherence to therapy, antibody formation, malnutrition, or hypothyroidism may be considered as possible causes. Somatropin would not significantly affect antidiuretic hormone (ADH) levels, or cause dehydration or water retention.
- To promote the absorption of regular insulin, one anatomic area should be selected for subcutaneous injections. Serial locations within that anatomic area are then chosen to rotate the exact injection site. Injection sites should not be rotated by using different anatomic areas each day, because this would substantially change the absorption of the insulin and the patient’s blood glucose levels. Using one injection site regularly may lead to lipodystrophy. Regular insulin is administered about 30 to 60 minutes before eating a meal, not after.
- Taking aspirin with milk or food minimizes the stomach upset because it buffers the stomach wall from direct contact with the medication, decreasing gastric distress. Chewable tablets can be chewed before swallowing or crushed and then advised to be taken with food or mixed in a drink. Swallowed whole, extended- release tablets are enteric coated to delay release of the aspirin, which again buffers the stomach wall from the medication, decreasing gastric distress.
- A nurse is caring for a 61-year-old man who has had a severe attack of gout while in the hospital for food poisoning. The nurse administers colchicine intravenously in order to
- The patient is given colchicine intravenously to avoid aggravating his gastrointestinal tract. Giving the drug intravenously may ensure quick distribution of the drug, but considering the patient’s food poisoning, the main objective would be to avoid aggravating the gastrointestinal tract and symptoms that the patient already has. Giving the drug intravenously does not prevent infection, bleeding, or depressed bone marrow function.
- The nurse will need to caution the patient about the adverse effect of photosensitivity, especially considering his work. He should be advised to wear protective clothing and sunglasses and to use sunscreen whenever he is outside on the job site. A complete blood cell count should be done before therapy begins but would not be needed again unless indicated. A nurse must check with the prescriber before advising a patient to decrease a drug dosage. A diet high in protein is not necessary with this drug.
- Aspirin has been associated with hepatotoxicity in patients with juvenile arthritis, active systemic lupus erythematosus, rheumatic fever, or preexisting hepatic impairment. The hepatotoxicity is thought to be a direct toxicity to the liver and is associated with high-dose therapy. Bronchoconstriction is one of the hypersensitivity responses to aspirin, while patients with hemophilia are at risk for agranulocytosis and aplastic anemia.
- General skin assessment, diet, and environment are also factors that need to be assessed, but these are not as important as assessing the patient’s nasal passages.
- Glatiramer should reduce the frequency of multiple sclerosis–related attacks and therefore decrease fatigue. Fatigue, weakness, spasticity, balance problems, bladder and bowel problems, numbness, vision loss, tremor, and vertigo are the most common symptoms of multiple sclerosis. Chest pain, breathing difficulties, and heart palpitations are all identified side effects of glatiramer and are not common manifestations of MS.
- The nurse must consider the patient’s dietary habits because foods high in purines increase uric acid concentrations in the blood, making a gouty attack more likely. Assessing the patient’s work environment, fluid intake, and ethnicity are not as important as assessing his dietary habits.
- High consumption of meat products and seafood increases the risk of hyperuricemia, which is the root cause of gout. Purine-rich vegetables do not increase the risk of hyperuricemia, and a high dairy intake is actually protective.
- Use of illicit drugs as well as an age-related decrease in renal function may have predisposed the patient to nephrotoxicity. Therefore, it is most important for the nurse to advise the patient to drink enough water to decrease the risk for nephrotoxicity when taking methotrexate. Avoiding red meat or taking the tablets before bedtime does not help reduce the risk of nephrotoxicity.
- While it is important to monitor a patient for nausea and vomiting and help him or her into a more comfortable position, it is most important to administer supplemental carbohydrates as soon as the patient becomes conscious.
- Taking vitamin B every day will help decrease the potential for adverse effects of methotrexate. This drug is given cautiously to very young and elderly patients, because these patients’ livers and kidneys cannot adequately clear the drug. Vitamin C is contraindicated with most antiarthritic and antigout drugs because it decreases the renal excretion of drugs. Supplements of vitamin A or D would not be necessary.
- Since administration of glatiramer is by subcutaneous injection only, the nurse will teach the patient to rotate injection sites. Appropriate sites for the patient would include the thigh, stomach, and upper arm.
- The most common adverse effects of allopurinol include pruritus, maculopapular rash, nausea and vomiting, elevated liver function tests, and acute gout symptoms. Blood sugar levels, blood pressure, and body temperature are not associated with adverse effects of allopurinol.
- After an early morning dose of NPH insulin, the patient should be alert for a possible hypoglycemic reaction during mid- to late-afternoon. The lengthy peak action time produces additional risks for hypoglycemic reactions.
- All of the patient’s adverse effects should be addressed by the nurse. However, the most critical effect that needs immediate attention would be the increased blood glucose. Drug therapy for the increased blood glucose may need to be altered. The patient should monitor blood glucose levels carefully and report abnormal findings as soon as possible. Medication can help his dry eyes, and a dose adjustment with the dextroamphetamine may be necessary if the jitteriness is profound and does not subside. Sympathomimetic action of the dextroamphetamine may lead to an inability to ejaculate and either increased or decreased libido. The patient and his partner may need to seek counseling for this concern.